If you place a medical device on the market your company must comply with the relevant legislation and corresponding processes.
In order to gain access in Europe your company must follow the current European Commission framework which is composed of three directives:
- Council Directive 90/385/EEC on Active Implantable Medical Devices (AIMDD) -1990
- Council Directive 93/42/EEC on Medical Devices (MDD) -1993
- Council Directive 98/79/EC on In Vitro Diagnostic Medical Devices (IVDMD) -1998
Latest modification of these three main directives have been by the directive 2007/47/EC in 2007.
 The European Commission is in the process of drafting new regulations to govern the regulation on medical devices and in vitro diagnostic medical devices in Europe that would be combined to form the medical devices regulation, and the in vitro diagnostic medical devices directive would be changed to the in vitro diagnostic medical devices regulation.
The European Commission is in the process of drafting new regulations to govern the regulation on medical devices and in vitro diagnostic medical devices in Europe that would be combined to form the medical devices regulation, and the in vitro diagnostic medical devices directive would be changed to the in vitro diagnostic medical devices regulation.
The urgent need to modify the directive should ensure:
- simplification of legislation to make it more understandable and user-friendly
- coherence and uniformity in the interpretation and implementation of the legal requirements in order to remove national variation
- innovation-friendly approach to made regulation more robust to future technologies
- review and consolidation of sectoral legislation to identify where action is needed
The public’s confidence in receiving safe, effective and innovative devices had significantly dropped since the first implementation of the European legislation over twenty years ago because the EU has grown largely in size, and technological and scientific advancements have rendered it harder to keep a clear overview of the production and distribution of compliant medical devices.
Parallel, the necessity to adapt to a growing global market made it apparent that the old framework, despite its various amendments over the years, needs to be updated. Various authoritative bodies of the EU member countries have joined in public consultations to discuss the general principles and minimum standards for consultation of interested parties by the Commission that need to be applied; responses were taken into account.
The goal was not to completely revise the current framework, but rather to change the directives which have been inconsistently amended and changed over the years, into newer, more specific guidelines that would support a more unified approach to manufacturing and distribution of medical devices throughout Europe.
Besides the profits for patients in regards to safety, manufacturers of medical devices would benefit from having a better traceability throughout the supply chain with the help of a unique device identification (UDI) system that enhances post-market safety of medical devices, reducing the probability of counterfeit devices that would be produced and sold on the market which leads hence to better supply chain security.
Additionally, the new guidelines would help to align with international guidelines, which would facilitate international trade, as stated in the press release from September 26, 2012.
An effective supply chain system ensures the safe delivery of intact, efficient products to the end-user. From the beginning of a device’s implementation, to production, delivery and shipment, many risk areas may arise that can render it unsafe or even deadly to the patient.
Unlike the flaws in the production process of medicines, which can include false handling of API’s, design and packaging errors, supply chain needs to focus on the risks in system transfers, storage and shipment conditions.
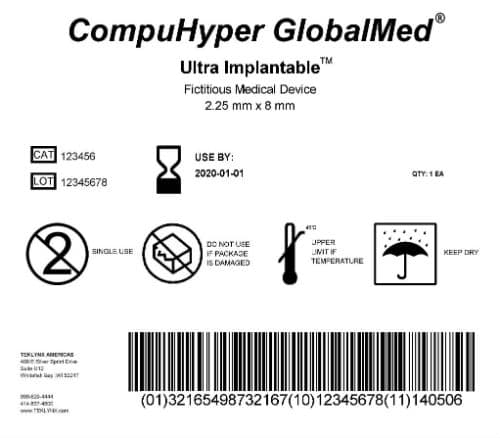
The risk to traceability for supply chain operations in pharmaceutical companies shall be mitigated with the implementation of UDI’s (Unique Device Identification). UDI’s adequately identify medical devices through their distribution and use and hence shall help ensure a more vigilant approach to tracing products, increase surveillance on individual packages throughout Europe and facilitate product recalls, while diminishing counterfeit products in circulation.
By placing vital information about the device (unique number and barcode identifier, the device’s manufacturer information, expiration date, etc.) directly on every device, it helps to make information publicly transparent, which serves as reassurance for the public because that information is made available in a public accessible database.
This kind of system has already been put to use in America, with the FDA expecting every device manufacturer to implement the UDI for all classified and unclassified devices by 2020, seven years after the final ruling.
If the above described actions are done successfully, this revolutionary plan can enable a ‘ship-to-order’ approach (much like online shopping) would not only benefit supply chain in having a clearer, up-to-date information, but also would communicate with the patient or professional health care provider on availability, recall information, and location of a device besides many other criteria needed for wholesome decision making.
A downside to the implementation of UDIs is that agencies would need to be accredited by the health authorities to be able to issue UDIs to manufacturers. This might result in higher costs for distributors, which then could be relayed to customers as a cost effective solution which would have to be invented to protect the customer and the supplier.
While the new regulations most and foremost bring along the change of increased and clearer vigilance and market surveillance, many steps still need to be taken to ensure this engagement to fully and sustainably align with all regulatory guidelines and compliance standards.
It is crucial to have a specific, unmistakable process in order to implement not only UDIs but also to regulate the processes for the entire European market to level the same standard of understanding and quality throughout.
Author: KVALITO Consulting Group





